|
After you've had your new bundle of joy for a few weeks (or more precisely 6) you will have your "postpartum checkup". If all is well, your OB will clear you for exercise and sex. Two things that probably couldn't be further down on your list of priorities. But that won't be the case for forever. When intimacy starts to look appealing again, it's important to know your options for birth control if avoiding another pregnancy is important to you and your partner. We've all heard conflicting pieces of advice about breastfeeding and return of periods after birth. It can all be boiled down to one sentence: Breastfeeding is designed to suppress ovulation, What factors? Well there are many. Some we can control, like rooming in with your baby and pacifier use - some we can not, like your unique threshold of Prolactin (the nursing hormone) to Follicle Stimulating Hormone and Estrogen (the menstruating hormones). While on average we see 6 months of ovulation suppression with exclusive breastfeeding, that first ovulation (and therefore menstruation) can come any point from 4 weeks to 2 years after birth while breastfeeding. That's a pretty big window! While OB's are happy to write a script for the mini pill (progestin only birth control pills, the only "approved" hormonal contraception for breastfeeding), many moms want to steer clear of hormones while nursing. And clinically speaking, as a lactation counselor, I've seen even the mini pill affect milk supply. So what's a mom to do?
The good news is that ovulation and that first menses after birth don't have to be surprise visitors. From 4 weeks to 2 years, you can track your fertility to know when your hormones start to rev up again. If you aren't already familiar with Fertility Awareness Based Methods, I would recommend working with a certified FAM Practitioner. If you have absolutely no idea what I'm talking about, you can learn more here. Even if you are using barrier methods in the meantime, or any method that doesn't actively interfere with ovulation, it's nice to have a window into knowing what the heck is going on.* Technology in this field has advanced so rapidly in the last 15 years, there are so many options to make Fertility Awareness Charting easier and more seamless. There are a few obvious ways to know your hormones are kicking in gear. Sex Drive That's right - just the moment you start to think sex sounds appealing, it's likely that is coming from Estrogen, one of the main drivers of female sex drive. Estrogen is second in line of the hormones that kickoff ovulation. Meaning when estrogen gets to a certain threshold, it pings to the brain to make Luteinizing Hormone, which officially kicks off ovulation. I joke with my clients that if you feel interested in sex, it's probably related to potential fertility. I haven't figured out the punch line to this joke yet. Cervical Fluid I usually give my spiel here about how Cervical Fluid is literally the substance of life, if men had it they would be bragging about it in bars, etc etc. Cervical Fluid, other than being the substance of life, gives us a direct line to our ovaries. It tells us everything we need to know about estrogen and progesterone production. What does this mean? It means when you are producing estrogen, and probably feeling a little hot and bothered to boot, you will see an increase in cervical fluid production. Yea, that stuff on your underpants. Cervical fluid production changes vastly in the postpartum period, and you can go months producing it without it leading to ovulation. FAM Practitioners are able to help you learn the language of your own cervical fluid to figure out what's happening. Sometimes learning that language is tricky, especially for those who didn't chart before baby. So that's when we lean on technology to help us... Hormonal Testing There are gadgets and gizmos these days to just test your hormones with at home urine tests. I know it doesn't sound sexy, but it gets the job done. Hormonal Monitors tell you when that Estrogen production is actually going somewhere. It also tells you when there are days that are completely infertile. (Good evenings to get the kids to bed early.) I'm still waiting for the toothbrush that just reads your hormones and gives you a full report directly to your cell phone. While we wait for that, Elon Musk, we'll use these primitive urine tests in the meantime. Birth control is an extremely personal issue. But if you want to avoid hormones while nursing, and even if you are using non hormonal forms like barrier methods, you can track your hormones so that first period after birth does not have to be a surprise. (Doesn't parenthood have enough surprises??) If you want to use Fertility Awareness Based Method for family planning intentions, I would recommend working with a FAM Practitioner. Be in the know and understand that wild hormonal postpartum ride just a little bit more! *If you are on any form of hormonal contraception, including the hormonal IUD, shot, or implant, you can not use a Fertility Awareness Based Method as they work primarily by suppressing the hormones that kick start the ovulation/menstrual cycle.
4 Comments
A woman in her mid-twenties who begins using a Fertility Awareness-Based Method (FABM) for charting or family planning will find it pretty straightforward. Ovulation is clear, and it’s easy to see the patterns emerging through her biomarkers in her cycles that tell her what’s going on hormonally.
Other periods in a woman’s life, however, such as puberty, postpartum, and perimenopause, can be a really tricky time to understand what’s going on. That’s because when a body is regulating (or in perimenopause’s case, deregulating), it is going through a period of transition. It’s sort of like fall or spring. You could be breezy and wearing flip-flops one day, and then needing a turtleneck sweater the next. It can be unpredictable and difficult to follow. Luckily, there are things we can be on the lookout for and there are ways to support a woman in perimenopause with the help of Fertility Awareness-Based Methods. With the right guidance, a prioritization of endocrine health, and a positive outlook, charting during this season doesn’t have to be quite so complicated. What’s going on? First off, let’s talk about what’s actually happening during perimenopause. This season could be compared similarly to puberty—but on the flip side. Instead of ovulation gearing up to be more regular, it is winding down to become less frequent and ultimately cease. Perimenopause can last a few months, or up to a decade. Each woman’s experience can vary, some experience the season intensely with side effects like hot flashes and sleep disturbances, while others experience nothing. Here is what’s going on “backstage” with the hormonal production: our bodies first start to create less progesterone. Then eventually less of the luteal hormone (LH). Then less estrogen and lastly, less of the follicle-stimulating hormone (FSH). This follows precisely the order, but backward, that hormones are produced chronologically in the menstrual cycle. In the beginning of perimenopause, the production of estrogen is higher than usual, as the follicles may need two, three, or more attempts to actually ovulate. If ovulation does occur, the progesterone is likely insufficient to counter the estrogen levels from prior. (Think of estrogen and progesterone as yin and yang—they balance each other out.) For a regularly cycling woman, we look for a 2:6 ratio of progesterone to estrogen. In perimenopause, they could double or triple, causing estrogen dominance. (This is in part what is responsible for those hot flashes!) Whenever a woman is in the perimenopause transition, I encourage them to get outside guidance from a Fertility Awareness-Based Method instructor. It’s hard to have your head in your own chart and be wrapped up in the details. Sometimes, getting a refresher course on what’s going on hormonally, helps you get out of your own chart just enough to get the right perspective. I often tell women to consider switching up their biomarkers if the ones they are reading aren’t clear enough. For example, if you’re only charting the signs of cervical mucus, think about adding a progesterone urine test or a Marquette monitor. These will give you just a little more insight into what’s going on. It’s likely you will have lots of days of cervical fluid in the beginning which will make charting confusing. If ovulation does occur, luteal phases may be short. Even though chances of pregnancy are much lower during perimenopause, if a pregnancy does occur, the mother has a higher chance of complications. If avoiding pregnancy is your intention, it’s important to take extra precaution. Other Important Considerations During this time and beyond, it’s crucial to prioritize endocrine health. Of course, there are obvious healthy lifestyle practices—like getting good sleep, eating whole unrefined and unprocessed foods, and participating in regular exercise—but during perimenopause, supporting your liver, gut, thyroid, and adrenal health are more important than ever. Many functional medicine doctors can provide you with tests (either blood or saliva) that can give you an idea of where you are on the spectrum or cycle deregulation. The tests can be paired, under the guidance of a medical professional, with bio-identical hormone therapy which is dramatically different than conventional hormone therapy. Bio-identical therapy is custom tailored to each individual’s needs. But this isn’t necessary for everyone. It’s most important that women take the time to care for themselves in the every day—in the little things. Perimenopause and postmenopause get a bad rap. While the body is certainly going through a lot of transitions, it doesn’t need to be as negative an experience as we often hear it described. Fertility Awareness-Based Methods can provide a helpful play-by-play of what is happening with your body, and there are nutritional and other adjustments you can make to improve your experience (see our Survival Kit for Perimenopause here!). Finally, during this season of life, women should take the time to pursue joy and the things that give them pleasure. A practice of prayer and meditation is helpful in stress management. And women usually find, on the other side, a whole new wisdom in their womanhood. This article was originally posted on 10/13/18 in Natural Womanhood. FEMM calls the spectrum of hormonal health The Continuum. It goes all the way from pre-puberty, into cycling, pregnancy, breastfeeding and past menopause. The phases are all part of the continuum but everyone's journey looks a little different. It might be completely normal for a woman to not ovulate or have irregular periods during a certain season. But what I like most about this concept is that it makes no assumptions about where a woman is and accounts for the fluidity of hormonal health.
I like to think of Family Planning intentions as a continuum, too. Sure, for some women, deciding whether or not to have a baby may be a definitive yes or no. But for many, it's more complicated than that. In the world of fertility charting you may have seen the acronyms (among many others) TTA and TTC. Respectively, trying to avoid (pregnancy) and trying to conceive. But a new acronym is finding its way into FAM bedrooms - TTW. Or trying to whatever. I have seen the fear based contraceptive culture that got us here - you can get pregnant anytime, anyway, anywhere - carried over into many fertility awareness discussions. Women get scolded in support groups for using a low risk day. (A day that is considered 100% fertile for TTA women, but only a little fertile for TTW women.) Any deviation from the strict rules of charting is paraded as an invitation for an unplanned pregnancy. And that's simply bad press, we can't have that. But are we in a place to judge a couple's decision to engage in risky days? Do we really know the full story? Consequently, efficacy rates of FABM are tricky to talk about. With pharmaceutical contraception, and particularly LARCs, your uterus is pretty well turned on or off. But Fertility Awareness methods are so much more nuanced than that. Using FAM allows you to be tuned in to the many factors that go into deciding (or not) to procreate. During a certain season of your life, you might not necessarily be aiming for a perfect efficacy rate. Baby making is biological, hormonal, situational, economical, and cerebral. In cases of difficulty conceiving and miscarriage, we don't always have complete control over our family planning. Do we allow for that fluidity in our discussions on birth control? I have wanted a baby so badly, been anxiety ridden during the two week wait (What was I thinking? A baby??) only to be crushed to find my period grace me with its presence. It's complicated. Boiling down the drive to procreate to an on/off button does a huge disservice to women and simplifies something that is anything but. Over the years I've practiced FAM, I've learned to be ok fluctuating on the spectrum. Communication with my partner (and myself to be honest) is uber crucial. Sincere, clear, down to the gut communication. But that can be difficult. It's easy to communicate "Yes, I'm fertile today." "No I'm not." What's not so easy to talk about is, "It's a low fertility day. What do you think? Are we ready to take that risk?" If it's a knee jerk reaction "Heck no," that's one thing, but the grey area often proves to be a challenge. In this sense, a couple using the fertility awareness method gets an opportunity for a valuable communication workout. In my work as a fertility awareness educator, I try to encourage this workout. It takes 2 to make a baby and there's 2 people with varying factors going into each cycle. If you don't get it out in the open to the other person, who might I add, has no other way of knowing what's going on - it might come out in another way. This isn't exactly the case for other forms of family planning and I think it's an important distinction to make. So wherever you are on the spectrum, be there. And there. And there, too. Process it, write about it, But most importantly, talk about it with the person who might be the other half of the decision. This makes using FAM different from other forms of family planning, but I have been pleasantly surprised by this element. Without it, I'm fairly certain I wouldn't have my daughter. This article was originally posted on 5/12/17 on Appleseed Fertility. It’s confusing growing up with a uterus and breasts. I have spent years studying and expanding my knowledge of the beautifully complex female reproductive system. These parts always felt mysterious and distinctly other from the rest of my body. After charting my cycles for 5+ years, dappling in Mayan Abdominal Massage, and venturing into v-steams, I have gained an appreciation for what my lower half can do. Pregnancy, labor, and delivery left me in awe of my own pelvic capabilities. And now, after breastfeeding for a year, my eyes have been opened to what those (not so) feeble A-cuppers are designed to do.
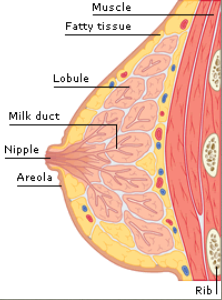
So when I was invited to attend a breast massage workshop hosted by Midwife, Massage Therapist, and Women’s Health Extraordinaire, Susanrachel Condon with the Earth + Sky team, I was delighted, if not also a little bemused. I thought, “That’s all good and well, I’m down for massage any day of the week, but how can we spend 6+ hours talking about rubbing boobs?” I was very quickly proven wrong. Breast massage includes work on the upper back, shoulders, and upper arm areas. All of course which are connected to the breast tissue in one way or another. The practitioner gave me a few options – she could massage on the skin like a regular massage, through a towel, or she could instruct and guide me to massage myself depending on my comfort level. (I opted for the full monty!) The lecture part of the class revealed so much on the anatomy, development and health of the female breasts. The same breasts I covered up in misfitted brasseries in 6th grade had a completely different cellular structure than the breasts I carried around in college, which were vastly different than the breasts I have been nurturing my daughter with for the last year. In short, the female breasts do not remain stable throughout a woman’s life. Their evolution is fantastically fluid. (No pun intended.) Between the ages of 17-24 the breasts develop the most alveoli they will ever contain (except for pregnancy). Through continual ovulation and production of high levels of hormones, breasts continue their life of prepping for lactation. Around the age of 35, there is a slow, but steady waning of hormones. The glandular development begins to decrease. This means that the mid-40’s woman’s breasts are less dense with less glandular and connective tissue. In other words, the breasts prepare for menopause a decade (or more!) beforehand. But don’t worry, the girls take their time, they shed aveoli slowly and thoughtfully. While on a cellular level, their composition is constantly evolving, so is their palpable quality. A woman may notice at one point in her cycle or season of life, they feel more or less lumpy. More or less sensitive. Or even painful. (Also known as Cyclic Mastalgia, which massage can help relieve.) They change in size. There are few nerve endings in breast tissue, but they respond very directly to estrogen and progesterone. So pain in the breasts, when not stemming from an infection or cyst, is usually referred from somewhere else in the body. It’s crucial that a woman knows her normal – even if that varies in a monthly menarche. Breast massage serves as a great starting point to familiarizing ourself with our breasts and starting the journey of healing our past with all the criticism that comes with growing up female. Some indications for breast massage include swelling in the lymph nodes from edema (raise your hands pregnant and postpartum mamas!). Massage can clear up general congestion and aid tenderness from fibrocystic tissue. As our breast undergo involution, either after weaning or approaching menopause, massage facilitates healthy drainage. It is also highly recommended for cancer patients. Women who have undergone surgery in the upper chest area, such as mastectomy or reduction, find massage helps immensely in the healing process. And lastly, it just downright feels therapeutic. You don’t need a medical reason to indulge in breast massage. In fact a little prevention can go a long way in keeping the girls happy and healthy. I left the class inspired and excited about all this new knowledge. I had discovered another hidden corridor on learning to delight in my female body. Breast massage felt like I was removing a bra I had been wearing for years and replaced it with a velvety cloak over my whole upper body. I feel like my relationship with my bosom has grown to be even more intimate, respectful, and loving. So the final verdict? Breast massage is a healing way to appreciate and maintain breast health. I am grateful that I was able to discover this lost art and I hope to carry it on to other women. So what do you say? Let’s #keepthegirlshappy (and healthy!) This was originally posted on 10/17/16 on Earth + Sky Healing Art's blog. |
Archives
May 2019
Categories |






 RSS Feed
RSS Feed